Does exercise help lower blood sugar? Yes, exercise is a powerful tool for lowering blood sugar. Regular physical activity plays a crucial role in managing blood glucose levels, especially for individuals with type 2 diabetes. But how exactly does breaking a sweat translate into better blood glucose control? Let’s dive into the science behind this vital connection.
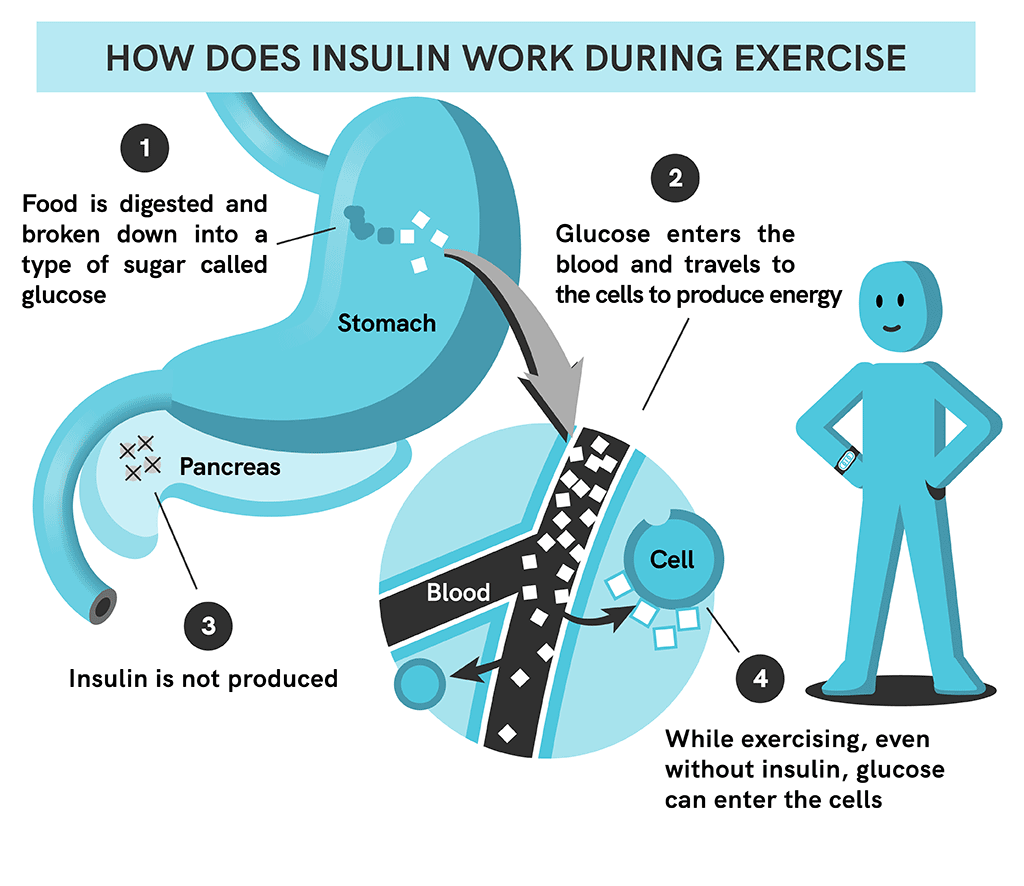
Image Source: wpcontent.glucare.health
The Body’s Glucose Regulation System
To grasp how exercise lowers blood sugar, we first need to understand how our bodies normally manage glucose. Glucose, a simple sugar, is our primary source of energy. After we eat, carbohydrates are broken down into glucose, which then enters our bloodstream. This rise in blood glucose signals the pancreas to release insulin.
Insulin acts like a key, unlocking cells to allow glucose to enter and be used for energy or stored for later. When insulin works efficiently, our blood sugar levels remain within a healthy range. However, in conditions like type 2 diabetes, the body either doesn’t produce enough insulin or the cells become resistant to its effects, leading to elevated blood sugar.
Exercise’s Direct Impact on Glucose
Exercise directly impacts blood sugar in several key ways, primarily by increasing glucose uptake by your muscles.
1. Enhanced Glucose Uptake by Muscles
During exercise, your muscles need more energy. To meet this demand, they actively draw glucose from your bloodstream. This process is largely independent of insulin, especially during moderate to intense aerobic exercise.
- Muscle Contraction: When your muscles contract during physical activity, they trigger signaling pathways that increase the number of glucose transporters (GLUT4) on the surface of muscle cells.
- GLUT4 Translocation: GLUT4 transporters act like doors, allowing glucose to move from the bloodstream into the muscle cells. Exercise promotes the movement (translocation) of these GLUT4 transporters to the cell membrane, even with less insulin present. This means more glucose is pulled out of the blood and used by the muscles for fuel.
- Post-Exercise Effect: This enhanced glucose uptake continues even after your workout has finished, a phenomenon known as the “exercise effect,” which can last for several hours.
2. Replenishing Muscle Glycogen Stores
Your muscles store glucose in the form of muscle glycogen. This is readily available fuel for your muscles during activity.
- Glycogen Breakdown: During exercise, muscle glycogen is broken down into glucose to provide energy for the contracting muscles.
- Replenishment: After exercise, your body works to replenish these depleted muscle glycogen stores. To do this, it needs glucose, which it draws from the bloodstream. This process also contributes to lowering blood sugar levels. The rate of replenishment is influenced by factors like the intensity and duration of the exercise, as well as post-exercise nutrition.
3. Improving Insulin Sensitivity
One of the most significant long-term benefits of regular exercise is its ability to improve insulin sensitivity. This means your cells become more responsive to insulin, allowing glucose to enter them more easily.
- Cellular Mechanisms: While the exact mechanisms are still being researched, it’s understood that exercise influences various cellular pathways involved in insulin signaling. This can include changes in insulin receptor function and the efficiency of downstream signaling molecules.
- Long-Term Impact: Consistent physical activity can lead to sustained improvements in insulin sensitivity, which is particularly beneficial for individuals with insulin resistance or type 2 diabetes. This means your body needs less insulin to move the same amount of glucose into cells, leading to lower overall blood sugar levels.
Types of Exercise and Their Blood Sugar Effects
Both aerobic exercise and anaerobic exercise contribute to lowering blood sugar, but they do so through slightly different mechanisms and with varying immediate and long-term effects.
Aerobic Exercise
Aerobic exercise involves sustained, rhythmic movements that increase your heart rate and breathing. Examples include walking, jogging, cycling, swimming, and dancing.
- Immediate Effects:
- Increased Glucose Uptake: During aerobic exercise, muscles rapidly consume glucose for energy, drawing it directly from the bloodstream. This leads to a noticeable drop in blood sugar during and immediately after the activity.
- Insulin-Independent Glucose Uptake: As mentioned, muscle contractions themselves promote glucose uptake via GLUT4 transporters, reducing reliance on insulin.
- Long-Term Effects:
- Improved Insulin Sensitivity: Regular aerobic exercise is a cornerstone for improving insulin sensitivity over time. This means your cells become better at responding to insulin, helping to manage blood sugar more effectively in the long run.
- Weight Management: Aerobic exercise is effective for burning calories and managing weight. Excess body fat, particularly around the abdomen, is linked to insulin resistance. Losing weight through aerobic exercise can significantly improve blood glucose control.
- Cardiovascular Health: Aerobic exercise also dramatically benefits cardiovascular health, which is closely linked to diabetes management. It helps lower blood pressure, improve cholesterol levels, and strengthen the heart, reducing the risk of heart disease, a common complication of diabetes.
- Increased Metabolic Rate: While the primary impact is glucose utilization, consistent aerobic training can also lead to a modest increase in your resting metabolic rate, meaning you burn more calories even at rest, aiding in weight management.
Anaerobic Exercise
Anaerobic exercise involves short bursts of high-intensity activity where your body’s demand for oxygen exceeds the supply, forcing it to produce energy without oxygen. Examples include weightlifting, sprinting, and High-Intensity Interval Training (HIIT).
- Immediate Effects:
- Glycogen Depletion: Anaerobic exercise heavily relies on muscle glycogen for quick bursts of energy. This leads to rapid depletion of these stores.
- Post-Exercise Glucose Uptake: Similar to aerobic exercise, the significant depletion of muscle glycogen during anaerobic exercise triggers an increased demand for glucose replenishment after the activity, leading to post-exercise glucose uptake.
- Hormonal Responses: High-intensity exercise can also lead to the release of hormones like adrenaline and growth hormone, which can mobilize glucose from storage. However, in the immediate aftermath of very intense exercise, there can sometimes be a temporary rise in blood sugar due to this hormonal response, which is then followed by a drop as the muscles begin to take up glucose for recovery.
- Long-Term Effects:
- Muscle Mass Growth: Anaerobic exercise, particularly strength training, builds muscle mass. Muscle tissue is metabolically active and uses glucose for energy even at rest. Having more muscle mass means your body can store more muscle glycogen and has a greater capacity to take up glucose from the blood.
- Improved Insulin Sensitivity: Studies show that anaerobic exercise also contributes to improved insulin sensitivity. The increased muscle mass and the metabolic adaptations within muscle cells play a role in this.
- Metabolic Boost: Building muscle mass can increase your resting metabolic rate, meaning you burn more calories throughout the day, supporting weight management and overall metabolic health.
Combining Aerobic and Anaerobic Exercise
For optimal blood glucose control and overall health benefits, a combination of both aerobic exercise and anaerobic exercise is generally recommended. This “mixed modality” approach leverages the strengths of each type of training for comprehensive health improvements.
Factors Influencing Exercise’s Effect on Blood Sugar
The extent to which exercise lowers blood sugar can vary based on several factors:
- Intensity and Duration: Higher intensity and longer duration workouts generally lead to a greater immediate drop in blood sugar. However, very prolonged or intense exercise without adequate fueling can sometimes lead to hypoglycemia (low blood sugar).
- Type of Exercise: As discussed, both aerobic and anaerobic exercise impact blood sugar differently.
- Time of Day: Exercising before a meal might lead to a more significant drop in blood sugar than exercising after a meal, as there’s more glucose available in the bloodstream.
- Hydration and Nutrition: Staying hydrated is crucial. Proper nutrition before and after exercise can also influence blood sugar responses and recovery.
- Medications: For individuals taking diabetes medications (like insulin or certain oral agents), exercise can increase the risk of hypoglycemia. It’s essential to consult with a healthcare provider about adjusting medication or timing of exercise.
- Individual Fitness Level: As you become fitter, your body may become more efficient at using glucose during exercise.
Exercise and Type 2 Diabetes Management
For individuals with type 2 diabetes, exercise is not just a helpful addition; it’s a cornerstone of effective management.
- Reducing Medication Needs: By improving insulin sensitivity and promoting glucose uptake, regular exercise can often help reduce the reliance on diabetes medications, and in some cases, even lead to remission.
- Preventing Complications: Managing blood sugar through exercise, alongside other lifestyle changes, is crucial for preventing or delaying the progression of diabetes-related complications, such as nerve damage, kidney disease, eye problems, and cardiovascular disease.
- Improving Quality of Life: Beyond direct blood sugar control, exercise enhances cardiovascular health, boosts mood, improves sleep, and increases overall energy levels, contributing to a better quality of life.
The Role of Insulin Sensitivity
Insulin sensitivity is central to how exercise helps manage blood sugar. When your muscles are more sensitive to insulin, they can absorb glucose more effectively, preventing it from accumulating in the bloodstream.
- Muscle Fiber Type: Different muscle fiber types may have varying responses to exercise in terms of insulin sensitivity.
- Fat Distribution: Visceral fat (fat around the organs) is particularly linked to insulin resistance. Exercise helps reduce this type of fat, thereby improving insulin sensitivity.
- Inflammation: Exercise has anti-inflammatory effects, and chronic inflammation is known to impair insulin sensitivity.
Exercise and Metabolic Rate
Your metabolic rate refers to the rate at which your body burns calories. Exercise influences this in several ways:
- During Exercise: Your metabolic rate significantly increases during physical activity as your body works harder to fuel your muscles.
- Post-Exercise: Even after exercise, your metabolic rate remains elevated for a period (the “afterburn effect” or EPOC – Excess Post-exercise Oxygen Consumption). This means you continue to burn more calories and utilize energy, contributing to better overall energy balance and potentially weight management.
- Long-Term Muscle Adaptation: As mentioned, building muscle mass through anaerobic exercise increases your resting metabolic rate, as muscle tissue is more metabolically active than fat tissue.
Practical Recommendations for Exercise
To reap the blood sugar-lowering benefits of exercise, consider these practical tips:
- Start Gradually: If you’re new to exercise, begin slowly and gradually increase the intensity, duration, and frequency.
- Consistency is Key: Aim for regular physical activity most days of the week. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity per week, plus muscle-strengthening activities at least two days a week.
- Listen to Your Body: Pay attention to how your body feels. If you experience symptoms of low blood sugar (shakiness, dizziness, sweating), stop exercising and check your blood sugar.
- Monitor Blood Sugar: If you have diabetes, monitor your blood sugar before, during, and after exercise, especially when starting a new routine or if you’re on medication.
- Hydrate: Drink plenty of water before, during, and after exercise.
- Consult Your Doctor: Always talk to your healthcare provider before starting any new exercise program, especially if you have diabetes or any other health conditions. They can help you create a safe and effective plan.
Frequently Asked Questions (FAQ)
Q1: How quickly does exercise lower blood sugar?
A1: Blood sugar levels can start to drop during and within an hour or two after exercise. The magnitude of this drop depends on the intensity and duration of the activity and your individual response.
Q2: Can I exercise if my blood sugar is too high?
A2: If your blood sugar is very high (e.g., over 250 mg/dL or 13.9 mmol/L) and you have ketones in your urine, it’s generally advised not to exercise. High blood sugar with ketones can indicate a dangerous lack of insulin. Exercise can sometimes worsen this. If your blood sugar is high but you don’t have ketones, light to moderate exercise might be appropriate, but it’s best to consult your doctor.
Q3: Will exercise lower my blood sugar too much?
A3: Yes, it’s possible to experience hypoglycemia (low blood sugar) with exercise, especially if you take insulin or certain diabetes medications, haven’t eaten enough, or exercise for longer than usual. Monitoring your blood sugar and being prepared with a fast-acting carbohydrate source (like glucose tablets or juice) is important.
Q4: How does swimming affect blood sugar?
A4: Swimming is an excellent form of aerobic exercise that effectively lowers blood sugar by increasing glucose uptake by muscles and improving insulin sensitivity. It’s also a low-impact activity, making it accessible for many.
Q5: What is the best time of day to exercise for blood sugar control?
A5: The “best” time can vary per individual. Some find exercising a few hours after waking up, before a meal, is effective. Others prefer exercising after meals to help manage the post-meal rise in blood sugar. Experiment and monitor to see what works best for you.
Q6: Does strength training or cardio lower blood sugar more?
A6: Both are beneficial. Aerobic exercise generally causes a more immediate drop in blood sugar during and shortly after the activity. However, anaerobic exercise (strength training) contributes significantly to long-term insulin sensitivity and increased muscle mass, which improves the body’s ability to manage glucose over time. A combination is often ideal.
Q7: Can exercise cure type 2 diabetes?
A7: While exercise can lead to remission in some individuals with type 2 diabetes, meaning blood sugar levels return to normal without medication, it doesn’t “cure” the underlying predisposition. Lifestyle changes, including regular exercise and a healthy diet, are crucial for managing the condition and preventing recurrence.
Conclusion
The science is clear: physical activity is a powerful ally in the quest for better blood glucose control. By enhancing glucose uptake, replenishing muscle glycogen, and most importantly, improving insulin sensitivity, exercise helps our bodies utilize glucose more effectively. Whether through aerobic exercise, anaerobic exercise, or a combination of both, incorporating regular movement into your life is a fundamental strategy for managing blood sugar, improving cardiovascular health, and boosting your overall metabolic rate and well-being, particularly for those navigating the challenges of type 2 diabetes. Always consult with a healthcare professional to tailor an exercise plan that suits your individual needs and health status.