Image Source: www.frontiersin.org
How Is Blood Flow Related To Lung Function During Exercise?
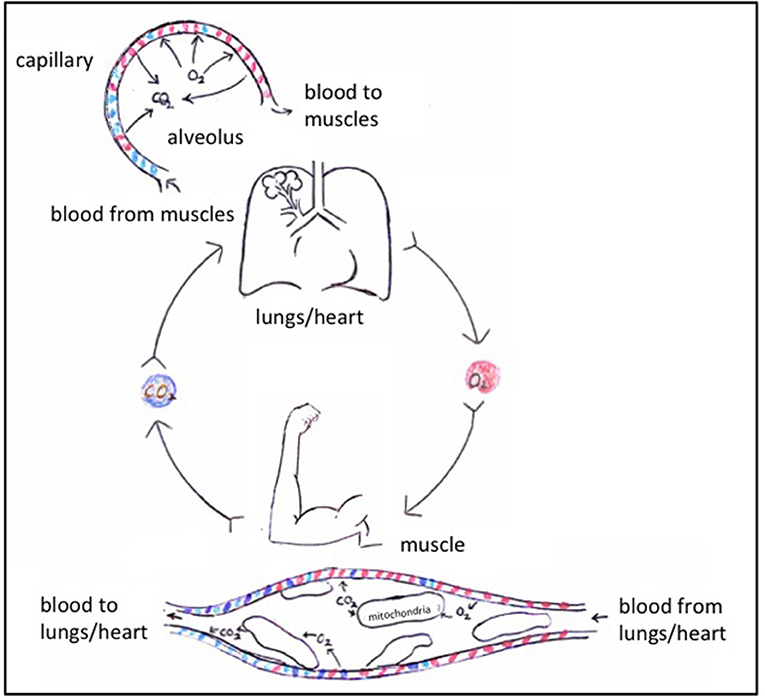
Blood flow is intimately connected to lung function during exercise, essentially acting as the delivery system that allows your lungs to do their vital job of getting oxygen into your body and removing carbon dioxide. What is this connection? It’s a dynamic partnership where the circulatory system (blood flow) and the respiratory system (lung function) work together to meet the body’s increasing demands for oxygen and to efficiently clear waste products.
The Crucial Role of Pulmonary Circulation
The pulmonary circulation is the specific pathway blood takes from the heart to the lungs and back again. This system is fundamental to how our lungs function, especially when we exercise. Think of it as a dedicated highway designed solely for the purpose of gas exchange.
Pulmonary Circulation Explained:
- Right Side of the Heart: Blood that has delivered oxygen to the body returns to the right side of the heart, specifically the right atrium and then the right ventricle.
- Pulmonary Artery: The right ventricle pumps this deoxygenated blood into the pulmonary artery. This artery then branches out, carrying blood to the lungs. It’s important to note that the pulmonary artery is unique because it carries deoxygenated blood, unlike most other arteries.
- Lungs and Alveoli: Within the lungs, the pulmonary artery branches into smaller and smaller vessels, eventually reaching tiny capillaries that surround the alveoli. The alveoli are the tiny air sacs in your lungs where the magic of gas exchange happens.
- Gas Exchange: Here, carbon dioxide, a waste product from your body’s cells, passes from the blood into the alveoli to be exhaled. Simultaneously, oxygen from the air you inhale passes from the alveoli into the blood.
- Pulmonary Veins: Now oxygenated, this blood travels back to the left side of the heart through the pulmonary veins. This is another unique aspect, as veins typically carry deoxygenated blood.
This constant loop ensures that your body’s tissues, especially your working muscles, receive a steady supply of oxygen.
Adapting to Exercise: A Symphony of Systems
When you start exercising, your body’s demand for oxygen skyrockets. Your muscles need more fuel to produce energy, and they produce more carbon dioxide as a byproduct. This is where the relationship between blood flow and lung function becomes particularly dynamic and impressive.
Increasing Oxygen Uptake
The primary goal during exercise is to increase oxygen uptake. This means getting more oxygen from the air into your bloodstream and then delivering it to your muscles.
How Blood Flow Facilitates Increased Oxygen Uptake:
- Increased Cardiac Output: Your heart pumps more blood per minute. This is achieved by increasing heart rate (how fast your heart beats) and stroke volume (how much blood your heart pumps with each beat).
- Vasodilation in Muscles: Blood vessels in your working muscles widen, a process called vasodilation. This allows more blood to flow into these active areas, ensuring they get the oxygen and nutrients they need.
- Redirected Blood Flow: Blood is preferentially shunted away from less active organs (like the digestive system) and directed towards the muscles that are working hardest.
- Enhanced Pulmonary Blood Flow: The pulmonary circulation also ramps up. More blood is pumped from the heart to the lungs, allowing for a greater volume of blood to be oxygenated.
This coordinated increase in blood flow directly supports the lungs’ ability to perform gas exchange more efficiently.
The Mechanics of Breathing and Blood Flow
Ventilation, which is the process of moving air in and out of your lungs, works hand-in-hand with blood flow.
Ventilation and Blood Flow Interplay:
- Breathing Rate: As exercise intensity increases, your breathing rate also increases. You take faster, deeper breaths to bring more oxygen into your lungs and expel more carbon dioxide.
- Alveolar Ventilation: This increased breathing leads to greater alveolar ventilation, meaning more air reaches the tiny air sacs where gas exchange occurs.
- Matching Ventilation and Perfusion: A critical concept here is the matching of ventilation and perfusion. Perfusion refers to the blood flow through the lungs. Ideally, the amount of air reaching the alveoli should be matched by the amount of blood flowing past them. During exercise, both ventilation and perfusion increase, and they generally increase in a coordinated manner to maximize gas exchange.
When you exercise, the lungs work harder to take in more oxygen and get rid of more carbon dioxide. Blood flow is essential to bring the carbon dioxide to the lungs and carry the oxygen away.
Gas Exchange: The Core Purpose
Gas exchange is the fundamental process that connects blood flow and lung function. It’s the critical step where oxygen moves from the air in your lungs into your blood, and carbon dioxide moves from your blood into the air in your lungs to be exhaled.
Factors Influencing Gas Exchange During Exercise:
- Increased Surface Area: While the total surface area of the alveoli remains relatively constant, during exercise, more capillaries in the lungs become open and available for gas exchange. This effectively increases the surface area for diffusion.
- Steeper Concentration Gradients: As your body uses more oxygen and produces more carbon dioxide, the concentration differences between the blood and the air in the alveoli become larger. This creates steeper concentration gradients, which drive faster diffusion of oxygen into the blood and carbon dioxide out of the blood.
- Shorter Diffusion Distance: The walls of the alveoli and capillaries are incredibly thin, creating a very short distance for gases to travel. This thin barrier allows for rapid diffusion.
- Blood Velocity: While blood flow increases overall, the velocity of blood flow through the capillaries surrounding the alveoli is regulated. It’s fast enough to deliver a large volume of blood but slow enough to allow sufficient time for effective gas exchange.
This efficient gas exchange is what allows your body to sustain physical activity.
The Impact on Athletic Performance
The efficiency of the blood flow and lung function relationship directly impacts athletic performance. Individuals with a highly developed aerobic system can deliver and utilize oxygen more effectively.
Blood Flow and Lung Function in Athletic Performance:
- Aerobic Capacity: Aerobic capacity, often measured as VO2 max (the maximum amount of oxygen your body can use during intense exercise), is a key indicator of fitness. A higher aerobic capacity means your circulatory and respiratory systems can deliver more oxygen to your muscles, allowing you to sustain a higher intensity of exercise for longer.
- Endurance: Improved pulmonary circulation and the ability of the lungs to efficiently transfer oxygen contribute significantly to endurance. As an athlete trains, their cardiovascular system becomes more efficient at delivering oxygenated blood to working muscles.
- Recovery: The systems also play a role in recovery. Once exercise stops, the increased blood flow helps clear metabolic byproducts like lactic acid and transport oxygen to aid tissue repair.
A well-trained athlete will have a more robust and responsive system, allowing for greater oxygen delivery and utilization.
Physiological Adaptations to Exercise
Regular exercise leads to remarkable adaptations in both your circulatory and respiratory systems, enhancing the blood flow-lung function connection.
Adaptations for Better Blood Flow and Lung Function:
- Increased Capillarization: Muscles develop more capillaries, leading to better perfusion of the muscle tissue. This means more blood can reach the muscle fibers.
- Improved Cardiac Function: The heart muscle becomes stronger and larger, allowing for a greater stroke volume and thus higher cardiac output at a given heart rate.
- Enhanced Lung Volumes: While total lung capacity may not change dramatically, the efficiency of breathing can improve. The muscles involved in breathing (diaphragm and intercostal muscles) become stronger.
- Increased Red Blood Cell Count: Training can lead to an increase in red blood cells, which carry oxygen. This boosts the blood’s oxygen-carrying capacity.
- Greater Vasodilation Response: The ability of blood vessels to vasodilate in response to exercise stimuli becomes more pronounced, improving blood flow to active tissues.
These adaptations collectively contribute to a higher aerobic capacity and improved athletic performance.
Factors Affecting the Relationship
Several factors can influence how effectively blood flow and lung function work together during exercise.
Influencing Factors:
- Altitude: At higher altitudes, the air has less oxygen. This means the lungs have to work harder to extract oxygen, and the blood needs to be delivered more efficiently to compensate for the lower oxygen availability in the air.
- Environmental Temperature: Extreme heat or cold can affect blood flow distribution. In heat, more blood is diverted to the skin to help with cooling, potentially reducing blood flow to muscles. In cold, blood vessels can constrict.
- Fitness Level: As discussed, a higher fitness level means a more efficient system.
- Age: With age, lung capacity and the efficiency of the cardiovascular system can decline, affecting exercise performance.
- Health Conditions: Respiratory diseases (like asthma or COPD) or cardiovascular diseases can significantly impair the ability of the lungs and blood flow to meet exercise demands.
How Blood Flow Supports Lung Function
It’s not just about the lungs getting oxygen to the blood; blood flow is also crucial for the lungs’ own metabolic needs and for removing waste from the lung tissue itself.
Blood Flow’s Support for the Lungs:
- Nutrient Supply: The lungs, like all tissues, need oxygen and nutrients. Bronchial arteries supply oxygenated blood to the lung tissues themselves.
- Waste Removal: Blood flow helps remove metabolic byproducts from the lung tissue.
- Fluid Balance: The pulmonary circulation plays a role in managing fluid balance within the lungs, preventing fluid buildup that could impair gas exchange.
Measuring the Connection
Several methods are used to assess the interplay between blood flow and lung function during exercise.
Assessment Methods:
- Spirometry: Measures lung volumes and airflow rates, providing insights into ventilation.
- Arterial Blood Gases (ABGs): Measures the levels of oxygen and carbon dioxide in the blood, directly reflecting gas exchange efficiency.
- Cardiopulmonary Exercise Testing (CPET): A comprehensive test that measures oxygen uptake, carbon dioxide production, ventilation, and heart rate responses during exercise. It’s a gold standard for evaluating aerobic capacity and the interplay between the systems.
- Echocardiography and Cardiac MRI: Can assess heart function and cardiac output.
- Pulmonary Artery Catheterization: Can directly measure pressures within the pulmonary circulation.
The Importance of Efficient Perfusion
Perfusion is the flow of blood through the capillaries. Efficient perfusion in the lungs is vital for optimal gas exchange. During exercise, the body improves perfusion in the lungs in several ways:
- Increased Blood Volume: More blood is circulated.
- Opening of More Capillaries: The body recruits more capillaries within the lungs to become active, increasing the total area available for blood to flow past the alveoli.
- Improved Blood Pressure Regulation: The cardiovascular system adjusts blood pressure to ensure adequate flow to the lungs.
When perfusion is not optimal, for example, in conditions like pulmonary embolism where blood flow is blocked, gas exchange is severely compromised, leading to a drop in blood oxygen levels.
Breathing Rate and Blood Flow: A Dynamic Duo
Your breathing rate and blood flow are not independent. They influence each other to maintain homeostasis during exercise.
The Interdependence:
- CO2 Levels: As you exercise, your muscles produce more carbon dioxide. This increase in carbon dioxide in the blood is a major stimulus for increasing your breathing rate.
- Oxygen Delivery: The increased breathing rate ensures that the lungs are well-supplied with oxygen. This oxygen then readily diffuses into the blood, allowing the pulmonary circulation to transport it efficiently to the tissues.
- Heart Rate and Breathing: Often, your heart rate and breathing rate will increase in parallel during exercise. This coordinated increase ensures that oxygenated blood is delivered to the muscles at a rate that matches the body’s demand.
This synchronized response is crucial for sustaining exercise and maximizing aerobic capacity.
Frequently Asked Questions (FAQ)
Q1: How does exercise improve lung function?
Exercise doesn’t directly increase the size of your lungs, but it makes them more efficient. Your breathing muscles become stronger, and your body gets better at extracting oxygen from the air you breathe and delivering it to your muscles. This improves your aerobic capacity.
Q2: Can you have good lung function but poor blood flow for exercise?
Yes, it’s possible. Someone might have healthy lungs but a weak heart or poor circulation, limiting their ability to deliver oxygen to their muscles. This would restrict their athletic performance, even if their lungs are fine.
Q3: What happens to blood flow in the lungs during intense exercise?
During intense exercise, cardiac output increases significantly, and a larger proportion of this blood is directed to the pulmonary circulation to be oxygenated. Blood vessels in the lungs also widen (vasodilation) to allow for greater blood flow and more efficient gas exchange.
Q4: Does breathing faster mean more oxygen gets to my muscles?
Breathing faster and deeper increases the amount of oxygen entering your lungs (ventilation). This allows for more oxygen to be absorbed into your blood through gas exchange. However, the real limitation for muscles is often how well the blood can deliver that oxygen, which depends on blood flow and the heart’s ability to pump. So, while faster breathing helps, efficient blood flow is equally important for delivering that oxygen.
Q5: What is the relationship between VO2 max and blood flow to the lungs?
VO2 max, or aerobic capacity, is directly influenced by how well your body can transport oxygen from the lungs to the muscles. A higher VO2 max means your heart can pump more blood (cardiac output) and your pulmonary circulation is efficient at oxygenating that blood. Thus, improved blood flow to and through the lungs is a key component of a high VO2 max.